Abstract
Introduction: Benign neutropenia (BN) is a heterogeneous group of rare disorders, as compared to neutropenia in patients with underlying malignancy. Febrile neutropenia in children with BN is a frequent cause for admission for intravenous antibiotic administration due to the possibility of life-threatening infections. However, the majority of children diagnosed with BN experience a benign clinical course and may not require aggressive medical management each time they develop a fever. Scant data exist regarding the incidence of bacteremia in BN patients. The aim of this study was to assess the rates of bacteremia and other morbidities in a large patient population of children with BN.
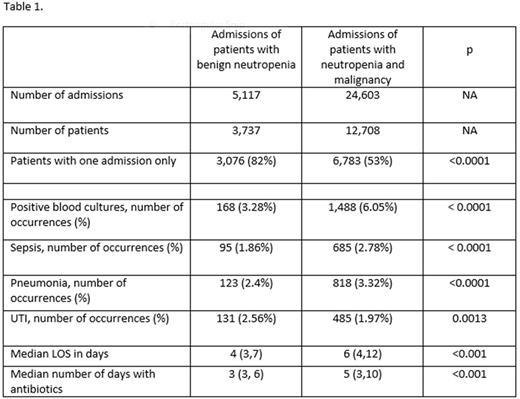
Methods: With IRB approval, the Pediatric Health Information System (PHIS) database was queried for children < 18 years admitted with fever and neutropenia between January 2011 and October 2015. The PHIS database captures de-identified patient information from 45 pediatric hospitals in the US. Patients were considered to have BN when identified with ICD9 codes for chronic, congenital, cyclic, genetic and immune neutropenia, and if they did not have a malignancy. Patients with neutropenia and underlying oncological diagnoses and who underwent HSCT served as controls. Bacteremia was identified using the ICD-9 diagnosis code (790.7). Infectious complications such as pneumonia, UTI and sepsis were also identified using ICD-9 diagnostic codes. The primary outcomes were admission rates, length of stay (LOS) and days of antibiotic use. The presence of bacteremia and other infectious complications was described with frequencies and per cents for each group and compared using Chi squared analysis or Fisher's exact test as appropriate. Continuous variables are described with medians and IQR and compared using Wilcoxon rank sum tests. LOS and days of antibiotic use were significant at the < 0.001 level. (Results are summarized in Table 1).
Results: There were a total of 29,720 admissions for febrile neutropenia: 24,603 of patients with malignancies, and 5,117 of patients with benign neutropenia. There were 16,445 unique patients, 12,708 with malignancies, and 3,737 without. Fifty three percent (6, 783) of the patients with malignancies had only one admission captured at a PHIS center during the study period, while 82% (3,076) of the benign neutropenia patients had only 1 admission. From the 24,603 admissions of patients who had malignancy and fever and neutropenia, 1,488 (6.05 %) occurrences of bacteremia were identified. There were 168 (3.28%) occurrences of bacteremia identified in 5,117 admissions of patients with benign neutropenia and fever. Pneumonia occurrences were identified as follows: in 818 (3.32%) admissions of patients with malignancy vs 123 (2.4%) admissions of patients with benign neutropenia. Sepsis was identified as follows: in 685 (2.78%) admissions of patients with malignancy vs 95 (1.86%) admissions of patients with benign neutropenia. UTI occurrences were identified as follows: in 485 (1.97%) admissions of patients with malignancy vs 131 (2.56%) admissions of patients with benign neutropenia. Median LOS for patients with benign fever and neutropenia was 4 (3,7) days compared to 6 (4,12) days for patients with malignancies. Median days of antibiotic use was 3 (3, 6) days in benign neutropenia patients vs 5 (3, 10) days in patients with malignancy.
Conclusions: In this large, multicenter database study we found very low rates of bacteremia both in patients admitted with fever and benign neutropenia and with neutropenia and underlying malignancy. The identified rates of pneumonia, sepsis and UTI were very low in both groups. The identified rates of pneumonia and sepsis were lower in patients with benign neutropenia and rates of UTIs were slightly higher in this group. Shorter LOS and shorter antibiotic courses were noted in patients with benign neutropenia compared with cancer patients. Further studies should explore the feasibility of outpatient management for febrile neutropenia in children with BN given the very low rates of bacteremia and infectious complications.
Ahuja: Bayer: Honoraria; Shire: Honoraria; Shire: Speakers Bureau; CSL Behring: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal